Mouth Cancer and Immune System Performance
In 2020, oral cancer was estimated to affect approximately 377,713 new cases and result in 177,757 deaths worldwide, ranking as the 13th most common cancer [1]. The immune system plays a significant role in the development, growth, and treatment of oral cancer, particularly oral squamous cell carcinoma (OSCC), through complex interactions within the tumour microenvironment (TME), immune evasion mechanisms, and response to therapies.
The TME in oral cancer is a complex ecosystem that includes cancer cells, immune cells such as T cells, B cells, macrophages, and stromal cells like cancer-associated fibroblasts (CAFs) [2][4]. CAFs secrete cytokines and growth factors that promote tumour growth, immune suppression, angiogenesis, and metastasis. Oral microbial pathogens, such as *Fusobacterium nucleatum*, associated with periodontal disease, can manipulate local immunity, rewiring immune cell behavior and promoting cancer progression and immune escape [1].
Immune evasion is common in oral cancer. For instance, human papillomavirus (HPV)-positive head and neck cancers, including some oral cancers, evade innate immunity by altering the interferon pathway, weakening antiviral defenses [2]. Mutations that impair immune signaling, such as in tumour necrosis factor receptor-associated factor 3 (TRAF3), further suppress immune responses [2].
Immunosuppression in the TME and factors like hypoxia contribute to resistance against radiotherapy and chemotherapy in oral cancer [2][4]. Immune recognition also affects the efficacy of advanced drug-delivery systems, as immune clearance can reduce therapeutic agent stability and bioavailability, hindering treatment effectiveness in OSCC [4].
Immune checkpoints (e.g., PD-L1) and signaling pathways such as NF-κB regulate immune responses to oral cancer. Studies show that enhancing immune responses by inhibiting PD-L1 expression or modulating pathways like IKK/NF-κB can improve outcomes [3].
The most common type of oral cancer is squamous cell carcinoma, accounting for around 90% of all cases. Common symptoms include sores, lumps, thick patches, white or red patches, difficulty chewing, swallowing, or speaking, pain or bleeding in the mouth, numbness, and ear pain [5]. HIV/AIDS, organ transplant medications, and aging can weaken the immune system, increasing the risk of oral cancer [5].
Oral cancers are more common in men and older people, with higher fatality rates observed in men compared to women [5]. The immune system works by telling the difference between cells that belong in the body and those that should not be there. Tumour-associated macrophages (TAMs), Treg cells, myeloid-derived suppressor cells, and tumour-associated neutrophils can promote cancer growth by suppressing the immune system's response to cancer [6].
The immune system ends an attack once the threat is over. It consists of two main parts: the innate immune system, which provides general defense, and the adaptive immune system, which is specific to certain germs and harmful substances [7]. The immune system is a complex system made up of multiple organs, cells, and proteins that work together to protect the body from harmful substances, germs, and changes in cells [7].
Cancer cells can release immunity-suppressing cytokines, causing immune surveillance to fail and allowing cancer cells to grow and spread. Immunotherapy can enhance the immune system's response to cancer, helping it recognise and attack cancer cells. Types of immunotherapy include monoclonal antibodies, checkpoint inhibitors, vaccines, cytokines, and CAR-T cell therapy [8].
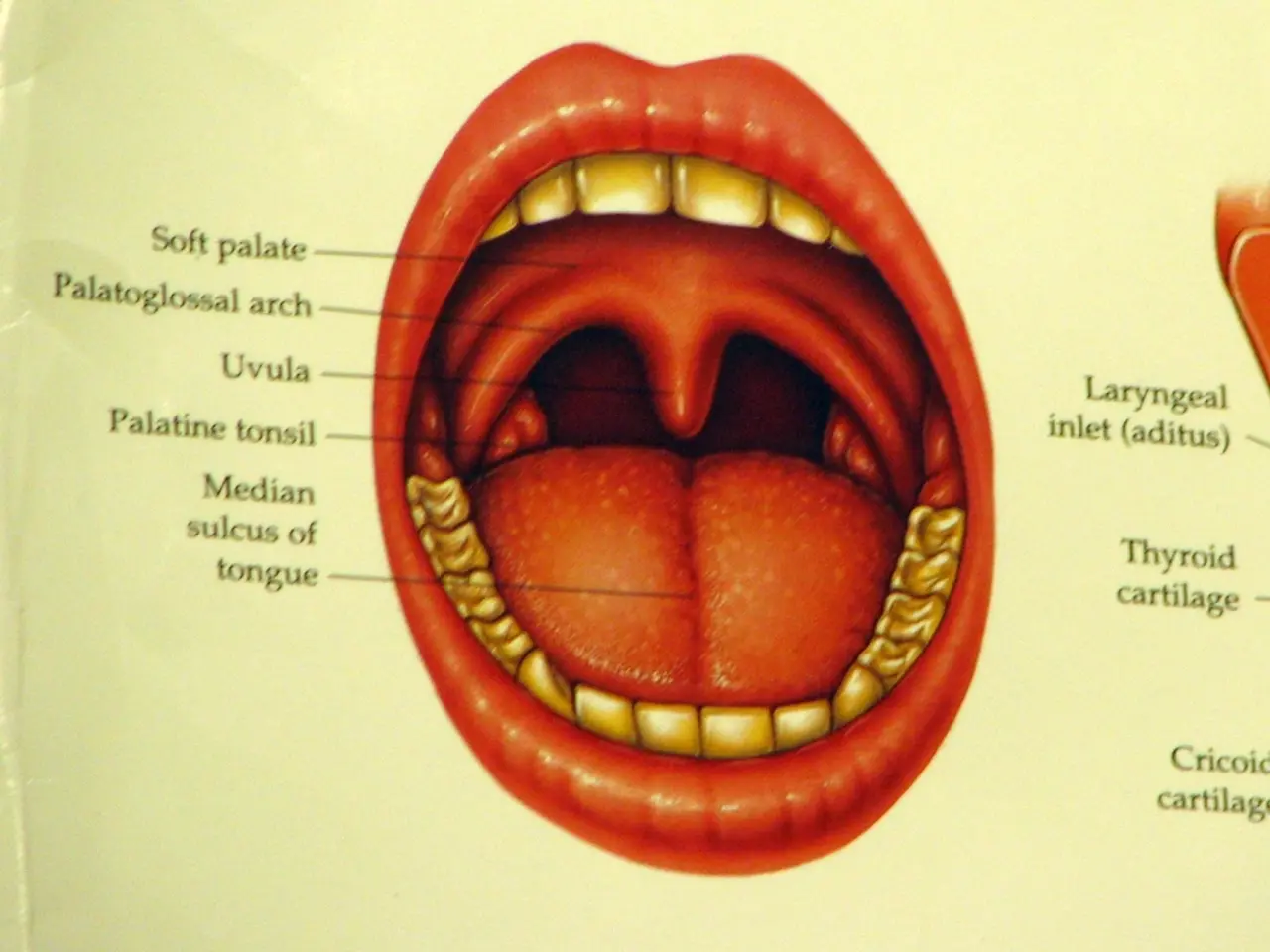
Tobacco use, betel quid chewing, alcohol consumption, a poor diet, mouthwash use, viral infections (such as Epstein-Barr virus, human papillomavirus, and herpes simplex virus), UV/sun exposure, radiation, genetics, and a weakened immune system are risk factors for oral cancer [9]. Oral cancer is a type of head and neck cancer that can develop in various areas of the mouth and oropharynx, including the lips, gums, tongue, buccal mucosa, floor of the mouth, roof of the mouth, retromolar trigone, oropharynx, and vestibule [9].
References: [1] Siegel, R. L., Miller, K. D., Jemal, A. (2020). Cancer statistics, 2020. CA: A Cancer Journal for Clinicians, 70(1), 7-30. [2] Chen, X., & Mao, Y. (2018). Immune microenvironment and immune evasion in head and neck squamous cell carcinoma. Cancer Immunology Research, 6(3), 290-303. [3] Wang, Y., et al. (2019). PD-L1 expression and its prognostic value in oral squamous cell carcinoma. Journal of Oral Pathology & Medicine, 48(4), e10. [4] Liu, Y., et al. (2019). The role of the tumor microenvironment in the drug resistance of oral squamous cell carcinoma. Oncotarget, 10(51), 9883-9899. [5] American Cancer Society. (2020). What are the key statistics about oral cavity and oropharyngeal cancer? Retrieved from https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/about/key-statistics.html [6] DeNardo, D. G., et al. (2014). The immune system in cancer: opportunities for immunotherapy. Journal of Clinical Oncology, 32(26), 2942-2952. [7] National Institute of Allergy and Infectious Diseases. (2018). The immune system: an overview. Retrieved from https://www.niaid.nih.gov/diseases-conditions/immune-system-overview [8] National Cancer Institute. (2020). Immunotherapy for cancer. Retrieved from https://www.cancer.gov/about-cancer/treatment/types/immunotherapy [9] American Cancer Society. (2020). What causes oral cavity and oropharyngeal cancer? Retrieved from https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/causes-risks-prevention/risk-factors.html
- Oral cancer, a significant health concern, is often influenced by the immune system's responses, as cancer cells can release immunity-suppressing cytokines, causing immune surveillance to fail and allowing cancer cells to grow and spread.
- Immunotherapy, a type of treatment, can enhance the immune system's response to cancer, helping it recognize and attack cancer cells, thereby improving health outcomes.
- Mental health is also relevant, as factors such as HIV/AIDS, organ transplant medications, and aging can weaken the immune system, increasing not only the risk of oral cancer but also other medical-conditions.
- Studies show that enhancing immune responses by inhibiting PD-L1 expression or modulating pathways like IKK/NF-κB can improve health outcomes in oral cancer, demonstrating the potential of science in cancer treatment.