Insights into Your Operating Room's Operations: A Glimpse from the Anesthesiology Residents' Point of View
In the heat of the operating room, sleep eludes many a perioperative team member. The OR, with its high patient acuity and intricate treatments, often lacks the tech-rich environment seen in other hospital areas. Anesthesiology, in particular, is a unique beast: one person shoulders the responsibility for their own checks and balances. These masters of medicine are tasked with a laundry list of tasks, each bearing the potential for error: determining appropriate medications and doses based on the patient's profile, checking for allergies and contraindications, sourcing meds from the storage area, prepping doses carefully, and administering them properly.
Armed with several meds at their fingertips, often without the safety net of electronic health records (EHR) or clinical decision support (CDS), anesthesiologists navigate a minefield of risk. While medication errors can potentially plague practitioners of any experience level, certain safety practices require targeted education and practice.
Our April 20, 2023 article, Ensuring competency and safety when onboarding newly hired professional staff - Part I, shed light on the fact that many healthcare practitioners, including anesthesiology residents, don't receive adequate training in vital topics like medication safety, medication-use systems, and basic prescribing, preparing, and administering meds.
When practitioners yearn to impress their supervisors and colleagues, they may hesitate to confess that they're uncomfortable with, or don't fully grasp, their tasks. This silence can lead to errors, potentially resulting in adverse patient outcomes. To intercept problems and avoid mishaps, anesthesia providers are expected to be transparent and empowered to "stop the line" when they suspect something is amiss. Yet, are organizations fostering an environment where staff feel secure enough to pause and ask questions before venturing into uncomfortable scenarios? Or do they find themselves in a bind where they must find solutions themselves, stalking through challenges and guessing to evade the specter of being deemed inadequate? Sharing and learning is crucial for continuous improvement. However, if a healthcare organization doesn't provide a psychologically safe space, practitioners may hesitate to challenge practices, share ideas, or report and learn from mistakes.
Below, we share incidents reported to ISMP that highlight issues commonly faced by anesthesia providers. We've enlisted the insights of anesthesiology residents who were not involved in these cases to help illuminate what may have contributed to these events.
Case #1: An attending anesthesiologist, overseeing a carotid artery surgery, instructed their resident to reverse the patient's neuromuscular blockade using "neo and glyco." Instead, the resident grabbed a syringe of NEOSYNEPHRINE (a former US brand name for phenylephrine) and administered it as an IV push. The patient's blood pressure skyrocketed to 300/150 mm Hg, and he began bleeding profusely from the surgical site, necessitating further intervention.
Case #2: During an intubation consultation on an inpatient medical unit, an anesthesiology resident directed a nurse to give the patient "30 of prop" for induction. When the attending physician arrived, they realized that the nurse had drawn up 300 mg/30 mL of propofol instead of 30 mg. Moderate hypotension ensued, but the mistake was caught before the full dose was administered.
From these cases, it seems that the anesthesiologist and residents may not have realized the risk of abbreviating drug names or using slang terminology. In Case #1, the resident might have shied away from seeking clarification from the attending due to feelings of inadequacy or fears of damaging personal trust. In Case #2, the resident may have adopted this habit from their mentors, using it when communicating with their anesthesia peers. It's crucial to be as detailed and clear as possible when communicating verbal orders, allowing—nay, requiring—the other practitioner to repeat back the order to ensure a shared understanding.
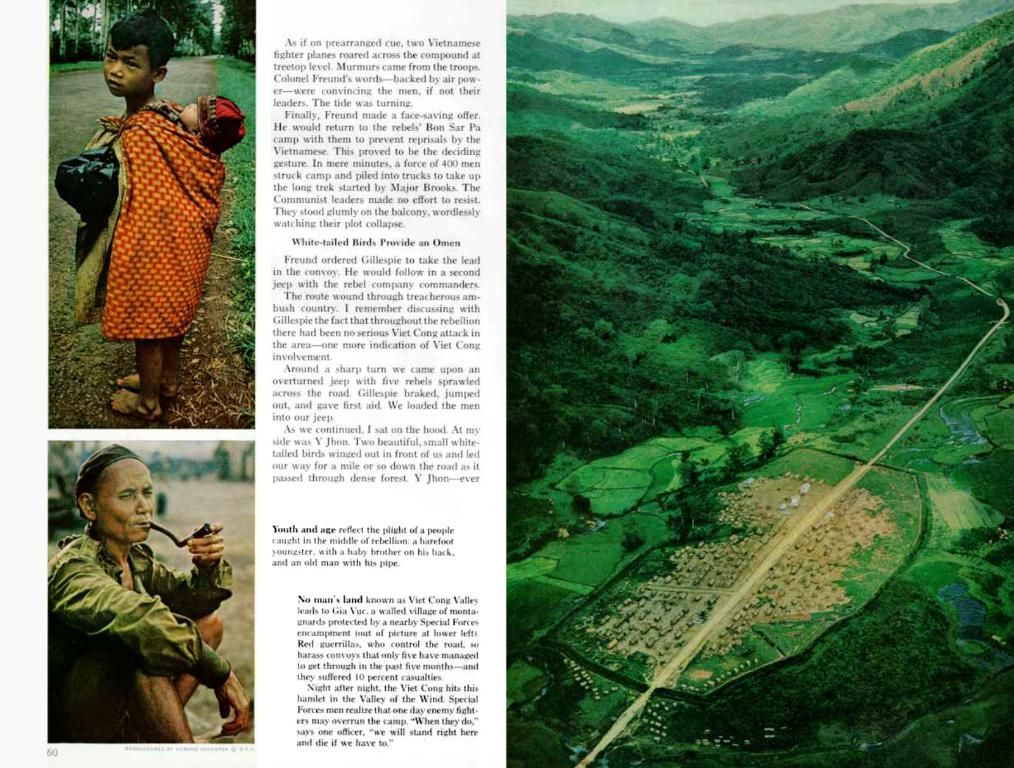
Case #3: In the middle of the night, a trauma patient arrived in the OR for an emergency thoracotomy. An anesthesiology resident placed a radial arterial line in the patient, and the procedure proceeded smoothly. During handoff, the ICU nurse identified that the arterial line pressure bag was spiked with a mannitol infusion rather than a 0.9% sodium chloride infusion. Both products, made by Baxter, come in 500 mL bags with black font that bears a striking resemblance to other infusion bags, such as Lactated Ringer's (Figure 1).
Case #4: For hydration, an anesthesiology resident planned to administer Lactated Ringer's to a pregnant patient prior to placing an epidural catheter. The resident removed the IV fluid tubing from the smart infusion pump to allow free flow at the highest rate possible. This, in turn, triggered uterine tachysystole, causing severe maternal pain and fetal bradycardia. The patient's nurse recognized that the resident had inadvertently initiated rapid hydration with the oxytocin infusion that had been started for labor induction. Terbutaline was required to arrest labor, and an emergency Cesarean section narrowly avoided.
In these instances, anesthesia providers face the challenge of distinguishing between medications and fluids that come in nearly identical packaging, setting them up for potential mix-ups. Along with similar-looking products, in many ORs the systems in place for barcode scanning of medication and fluids, as well as smart infusion pumps with dose error-reduction systems (DERS), aren't always utilized fully.
Case #5: A pregnant patient in labor who was receiving a BUPivacaine and fentaNYL epidural infusion was brought to the OR for a Cesarean section. The chief anesthesiology resident prepared and labeled doses of lidocaine and ceFAZolin in 20 mL luer lock (parenteral) syringes. The resident administered an epidural bolus of what they thought was lidocaine for pain relief. The patient began experiencing seizures, necessitating intubation with general anesthesia for an emergency Cesarean section and transfer to the ICU. Later, the resident identified that they had accidentally administered ceFAZolin instead of lidocaine epidurally. The patient experienced transient short-term memory loss, and there was no apparent harm to the neonate.
Preparing epidural medications using luer syringes is a widespread practice in the OR. Many hospitals have not yet embraced the use of NRFit connectors, the system designed to prevent neuraxial misconnections. NRFit connectors are 20% smaller in diameter than luer connectors and prevent medications intended for neuraxial administration from connecting with devices used for IV, enteral, and other applications, or vice versa.
Case #6: During a vascular procedure, a surgeon who had been practicing for years requested that an anesthesiology resident administer heparin. The surgeon, however, referred to the dose in mg rather than units. The resident didn't repeat the order, and instead prepared and administered the dose in units rather than mg of heparin. As a result, the patient experienced thrombosis due to the underdose.
Heparin is prescribed in units, not mg. The resident should have questioned the order with the surgeon, clarifying the dose in units, not mg.
To promote anesthesia safety and reduce errors, organizations should adopt these best practices:
- Elevate Medication Safety Awareness: Engage all perioperative team members in discussions about medication safety, standardize orientation processes, provide medication-specific education for critical tasks, assess competency skills, and knowledge, and employ simulation programs to ensure mastery of essential medication-related tasks.
- Proactive Safety Analysis: Assess new products for potential risks such as look-alike labeling and packaging concerns with other products in use. Reach out to manufacturers, ISMP, the US Food and Drug Administration (FDA), and healthcare purchasers when risks are identified.
- Maximize the Use of Commercially Prepared Products: Utilize ready-to-administer formulations and pharmacy-prepared syringes in the perioperative setting.
- Expand Barcode Scanning: Implement barcode scanning technology in short- and limited-stay locations such as perioperative and procedural areas to help curb look-alike packaging and labeling events.
- Label Practitioner-Prepared Doses: Always label all practitioner-prepared infusions and syringes with the drug name, concentration, and volume. Eliminate handwritten labels and incorporate machine-readable codes on medication labels, as well as preprinted sterile labels (or sterile blank labels and smudge-proof markers). When possible, have a second perioperative team member double-check the dose and volume with the label before administering the medication.
- Read Medication Labels: Carefully review individual product labels after removing the medication from the anesthesia tray, when removing infusions from overwraps, when spiking an IV bag, and prior to administration. When possible, employ audio/visual feedback to confirm the identity of the medication prior to administration.
- Communicate Doses Safely: Absolutely, positively refrain from using shortened or abbreviated drug names. Instead, stick to using the generic and/or brand name of the medication, and include an indication with medication orders to avoid confusion. Adopt closed-loop communication, where the recipient of the verbal order repeats back the precise medication dose (including units of measure). Enunciate each digit in the dosage to avoid misinterpretation. Question any medication-related concerns and consult with prescribers if a requested medication or dose doesn't fit the patient's condition. Ensure the mode of administration is always part of the order, as it should never be assumed.
- Make Use of DERS a Standard: Employ smart infusion pumps for all continuous medication infusions in the OR, as well as intermittent and secondary infusions, loading and bolus doses, patient-controlled analgesia infusions, epidural and nerve block infusions, and hydrating solution infusions (except when the hydration fluid administration rate exceeds the pump's capacity).
- Label and Trace Lines: Label all infusion lines at points of connection, double-check infusions and streams, and verify the proper infusion, pump/channel, and route of administration into the patient before starting the infusion.
- Encourage Open Dialogue: Foster a professional culture that empowers practitioners to voice their concerns and ask questions. For additional information, consult our March 10, 2022 article, Addressing Disrespectful Behaviors and Creating a Respectful, Healthy Workplace-Part II. Stress the need to confront doubts and avoid making assumptions. Encourage practitioners to ask questions and share their learning experiences in order to continually improve.
- Plan for NRFit Device Conversion: Follow guidelines from the Institute for Safe Medication Practices to transition to the ISO 80369-6 design standards for neuraxial (NRFit) connectors to minimize the risk of IV and neuraxial misconnections.
- Report Errors: Emphasize that the organization values a culture of safety and encourages medication error reporting and sharing of lessons learned. Consider establishing a program that includes "weekly shout-outs" or "good catches" to acknowledge practitioners who exemplify the principles of safety.
For the sake of our patients, let's make the OR a safer place. Let's speak up, let's speak out, and let's never stop learning.
- In the absence of electronic health records (EHR) or clinical decision support (CDS), anesthesiologists often navigate a tech-rich environment with multiple devices, relying on their own checks and balances.
- Medication errors are a potential risk in any healthcare practice, but anesthesiology requires targeted education and practice in medication safety, systems, and administration.
- Healthcare practitioners, including anesthesiology residents, may lack sufficient training in vital topics like medication safety and incômpétence in medication-use systems, which can contribute to errors.
- Anesthesia providers are expected to be transparent and empowered to "stop the line" when they suspect issues, but it's questionable whether organizations foster an environment that encourages staff to ask questions or challenge practices.
- Case #1 involved an attending anesthesiologist instructing a resident to reverse a patient's neuromuscular blockade using "neo and glyco," leading to the administration of the wrong medication neosynephrine instead of neostigmine.
- Case #2 demonstrates the risk of abbreviating drug names or using slang terminology, resulting in a nurse preparing and administering 300 mg of propofol instead of the intended 30 mg.
- Case #3 exemplifies the challenge of distinguishing between medications and fluids that come in nearly identical packaging, setting up anesthesia providers for potential mix-ups.
- Case #4 highlights the importance of carefully reviewing medication labels before administering them, as a resident inadvertently initiated rapid hydration with an oxytocin infusion instead of lactated Ringer's.
- In Case #5, a pregnant patient was administered ceFAZolin instead of lidocaine epidurally, underscoring the need for labeling all practitioner-prepared medications and reducing the use of handwritten labels.
- Case #6 illustrates the importance of enunciating each digit in the dosage and questioning any medication-related concerns to avoid confusion and errors.
- To promote anesthesia safety and reduce errors, organizations should employ best practices like standardizing orientation processes, utilizing barcode scanning technology, and labeling all practitioner-prepared infusions and syringes with the drug name, concentration, and volume.
- Open dialogue and a professional culture that empowers practitioners to voice their concerns and ask questions are crucial for continuous improvement and maintaining a safety-focused environment.